How to Prevent Ear Pain:
- Refrain from putting things into your ears such as cotton swabs, bobby pins, your fingers, etc. as this can cause damage to your eardrum and increase your chances of something getting stuck in your ear/eardrum.
- When blowing your nose, do it gently and one nostril at a time.
- Avoid smoke as much as possible. Smoking and secondhand smoke can increase your risk of infection.
- When swimming, wear earplugs and refrain from swimming in dirty waters.
 If you’re an adult and you happen to have an earache, try applying a warm washcloth or a heating pad next to your ear. You can also try the cold therapy method by applying a cold compress or ice bag next to your ear for 20 minutes. Be sure to take a pain reliever, such as an acetaminophen, aspirin, or Motrin (ibuprofen) to help with the pain and reduce inflammation. If nothing works, seek medical attention.
If you’re an adult and you happen to have an earache, try applying a warm washcloth or a heating pad next to your ear. You can also try the cold therapy method by applying a cold compress or ice bag next to your ear for 20 minutes. Be sure to take a pain reliever, such as an acetaminophen, aspirin, or Motrin (ibuprofen) to help with the pain and reduce inflammation. If nothing works, seek medical attention.To help open your Eustachian tubes and keep them drained, try the following:
Sleep with your head propped up
Chew gum – especially when experiencing pressure changes (i.e. during plane travel).
Stay awake during the ascending/descending of plane travel – this is when eardrums will plug up and cause pain. Try taking a decongestant a few hours before your plane ride as this will help prevent buildup in your nasal passages.
Try yawning to contract the muscles that open your Eustachian tubes.
Gently blow through your nose while holding both nostrils closed until you hear a pop. This helps promote ear drainage and can be done several times a day.
Take a decongestant when you get a cold and continue taking it until the cold is gone. Check with your doctor to see if it is ok for you to take a decongestant.
Take a hot shower – the steam will help to break up and soften earwax buildup.
In the case of children and earaches, usually they are brought on by an infection in the middle ear. This could be due to the fact that the Eustachian tubes are shorter and smaller in children.
How to tell if your child has contracted an earache:
- If you notice the ear seeping with fluid or excess ear wax.
- If your child begins pulling or rubbing his/her ear often, sometime your child will hold or cup his/her hand over the ear.
- If your child complains of any ear pain.
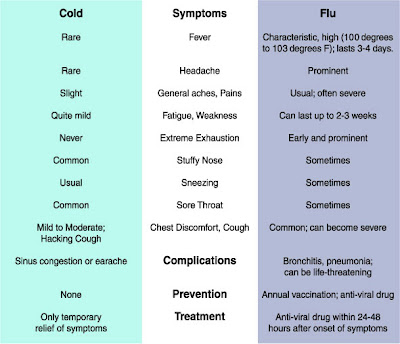
- If your child develops a fever.
- If your child becomes irritable.
- If your child has trouble hearing you.
- If your child suffers a sudden loss of appetite.
Make sure that your child finishes, in its entirety; the prescription of antibiotics to make sure that the bacteria has been destroyed. If your child has been seen by the doctor, and has taken medicine (usually antibiotics) for under two days and shows no signs of improvement you should visit your doctor again. Also if there is any swelling behind or around the ear, or if any drainage from the ear continues, you should contact your doctor again.